World Incontinence Week - Highlight on Urinary and Bowel Incontinence
24 June 2022
(Last updated: 24 Jun 2022 11:29)
 Urinary incontinence
Urinary incontinence
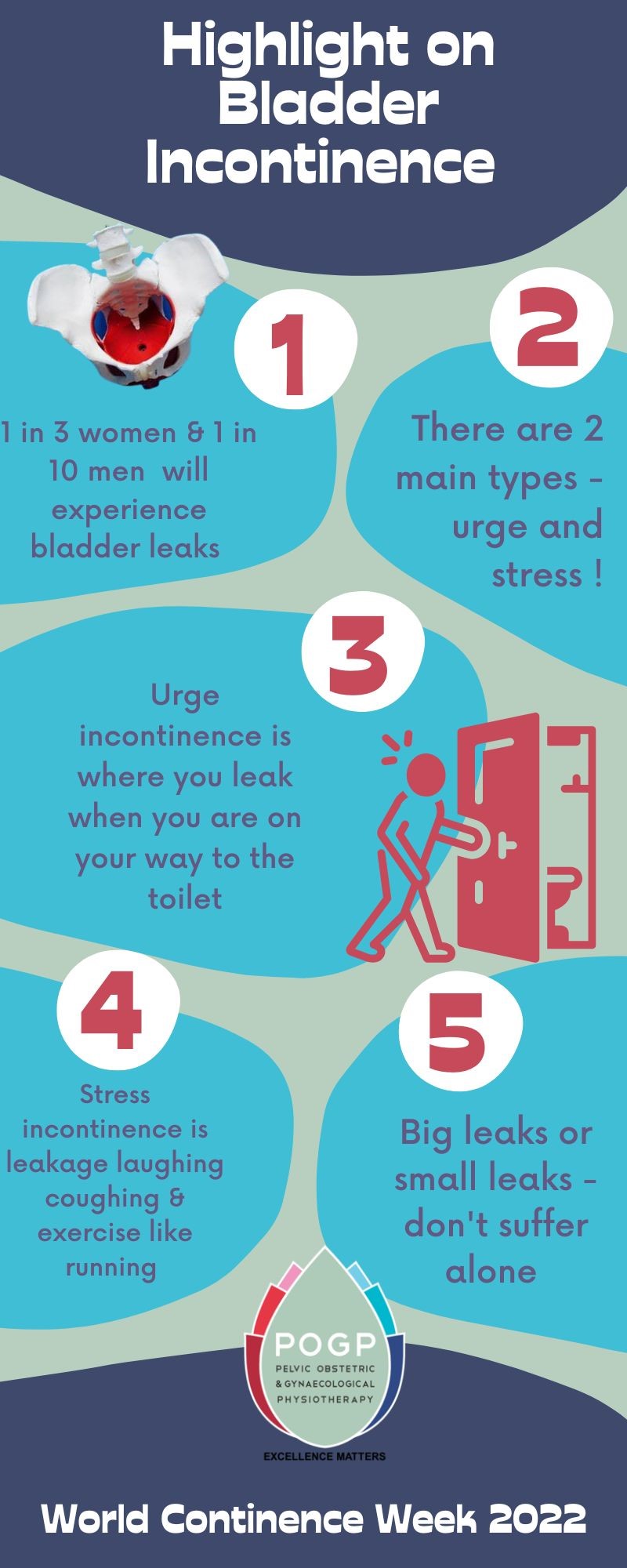
Urinary incontinence, or bladder leakage, is a common problem but not “normal because you’ve had children”. In the UK, 1 in 3 women will suffer bladder leakage, affecting millions of people.
You might leak when you sneeze or cough or with activity or you might leak just when you need a pee.
People live with urinary leakage making lifestyle changes such as using pads; wearing dark clothing; stopping exercise; and only going out if they know there will be a toilet.
They don’t tell friends and family and this is something we need to help change.
If you share your problem with a health professional the chances are your problem will be improved by more than a half. If you have an assessment and treatment with a Pelvic Health Physiotherapist you are likely to improve your leaking by 85%!
Management tips for urinary incontinence
Let’s clear up some terms and some management tips that can help:
- Stress incontinence occurs when the pelvic floor muscles are unable to maintain closure of the bladder tube when the pressure rises in the abdomen for example in coughing, sneezing lifting and bending over.
- Urge Urinary Incontinence tends to happen with a sudden sense of urgency and leaking occurs on the way to the toilet, in addition to triggers like turning on a tap, arriving home to put your key in the front door and feeling the cold.
Any type of incontinence should be discussed with a healthcare professional. It is also important to make sure if you have any symptoms of urinary tract infections to get these checked with your GP as infections can also lead to bladder leaking.
- Urinary incontinence can be affected by the things you drink, for example, drinking too much caffeine, alcohol and fizzy drinks.
- Not drinking enough makes your urine more concentrated and you need to pee more and may leak more. You should drink around 2 litres of fluids per day! The majority of this as water.
- Pelvic floor muscles can help with stress and urge incontinence leaks.
 Pelvic floor muscles
Pelvic floor muscles
Pelvic floor muscle exercises are known to help urinary incontinence and we have good evidence for this. They are an important set of muscles that need to be exercised like any other muscle in our body, think “use it or lose it”.
The pelvic floor muscles run from the pubic bone at the front and attach on to the tailbone at the lowest part of your back called the coccyx.
The muscles help the bladder and bowel openings to stay closed to prevent leaking. These muscles also need to be able to relax to help empty your bladder and bowel.
It is this ability to squeeze and relax that is the key to improving urinary incontinence. The muscles themselves should be able to freely go from squeezing to relaxing, picture the lovely movement that a jellyfish makes, lifting up and then letting go.
It is important to know if you are doing your pelvic floor exercise in the right way. Listen to this audio for women or this one for men on how to do these exercises correctly.
Once you can do these exercises try them lying, sitting: whatever feels easiest to you. A routine that mixes Slow and Fast squeezes is best. Start by holding for 5 seconds if you can and then relax and rest for 5 seconds. Repeat 5 times. Then try 10 fast squeezes. Try to do this routine 3 times a day.
Breathe normally throughout.
If you are unable to feel a squeeze it is worth seeing your GP to ask for a referral to see a Pelvic Health Physiotherapist who can help assess these muscles. We can’t talk about bladder leaks without mentioning the importance of keeping your bowels happy. Bowel issues are a classic silent problem causing misery in people’s lives.
Bowel incontinence
Everyone’s bowel pattern is different but we should be aiming for three to four bowel movements per week, your poo should be soft and easy to pass without straining.
Bowel urgency is when we need to rush to the toilet quickly to empty our bowels.
Bowel incontinence is when we leak wind, liquid or stool.
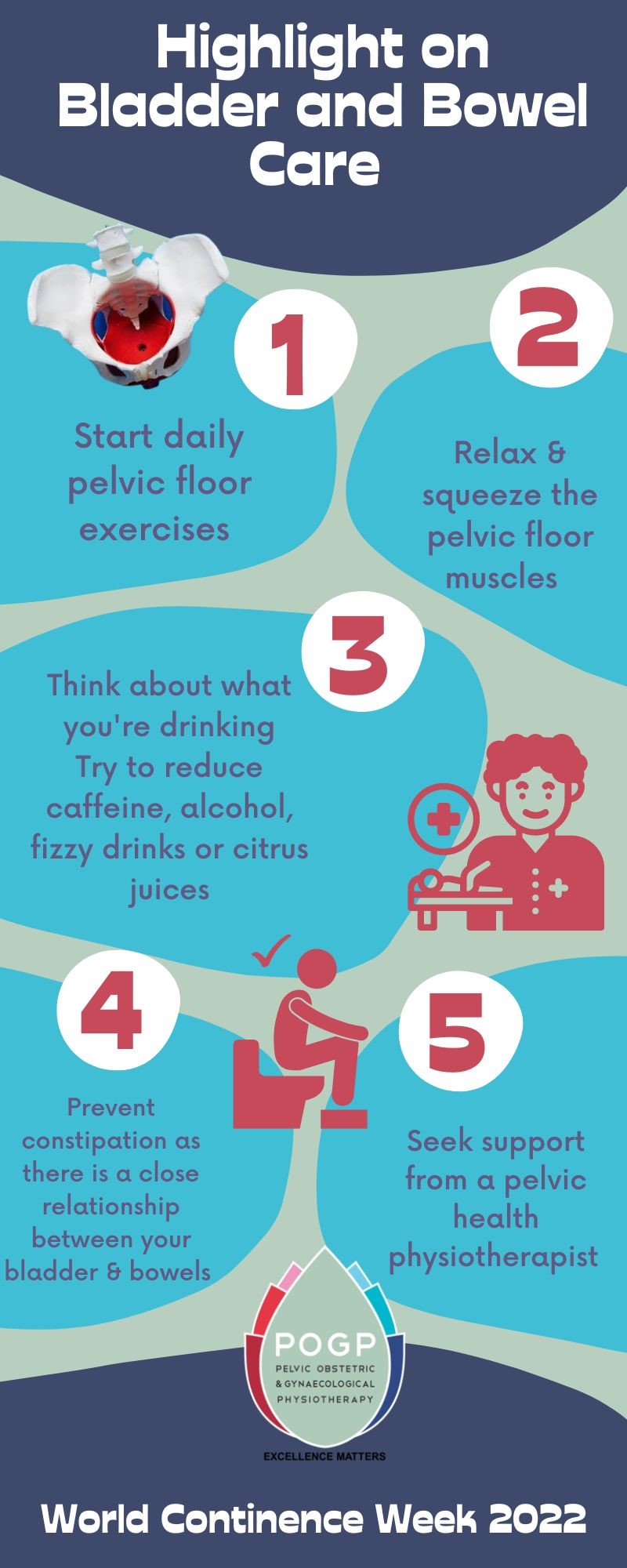 Just like the bladder, pelvic floor muscles help to control the bowels and prevent urgency and incontinence. If we are unable to lift and control the opening of the bowel, incontinence can occur.
Just like the bladder, pelvic floor muscles help to control the bowels and prevent urgency and incontinence. If we are unable to lift and control the opening of the bowel, incontinence can occur.
Bowel incontinence affects people of all ages, between 6% and 15% of the population, and tends to worsen with age. Bowel and urinary incontinence is estimated to occur in about 10% of women.
Regular or prolonged constipation, difficulties in emptying the bowels, struggling to control your stools, leakage, flatulence (sneaky gas), rectal prolapse, haemorrhoids, and pain from anal fissures are all reasons to contact a health care professional.
It’s quite difficult to chat to people about your bowel problems but a pelvic health physiotherapist can support you to improve your symptoms through conservative treatment.
Look at this 'Improving Your Bowel Function' leaflet here for more advice. If you need it in a different language or other accessibility features, use the red Recite me accessibility and language options button on the website.
View other News