Vaginal Prolapse
Explanation of common symptoms/ problems
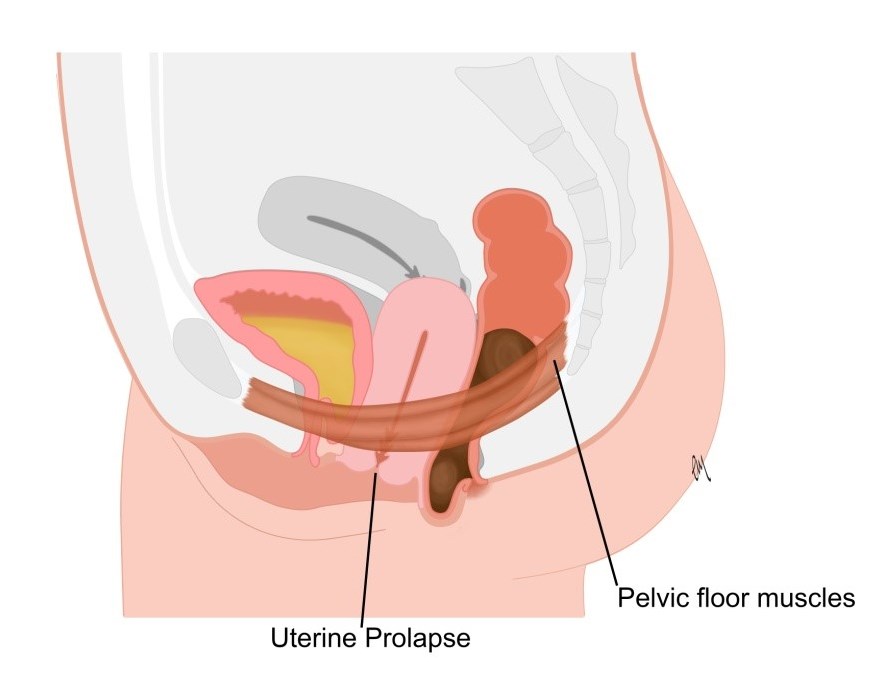
Vaginal prolapse (sometimes called pelvic organ prolapse) is when one or more of the vaginal walls or top of the vagina move downwards and cause a bulging or heavy feeling at the vaginal entrance. The bulge may stay within the vagina or beyond the vaginal entrance and feel like a small plum. If the top of the vagina is affected the uterus will sit lower in the vagina or may be felt just outside the entrance. Even if you have had a hysterectomy, the top of the vagina may still prolapse downwards.
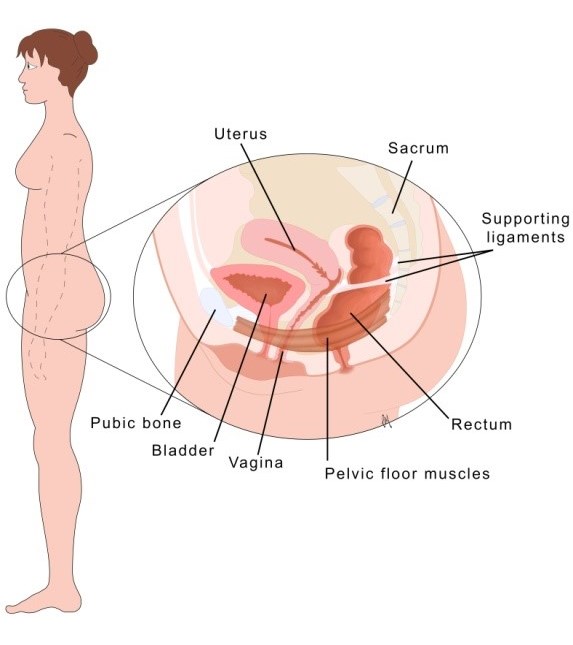
Picture of your pelvic floor muscles (below)
Picture of an anterior wall prolapse (below)

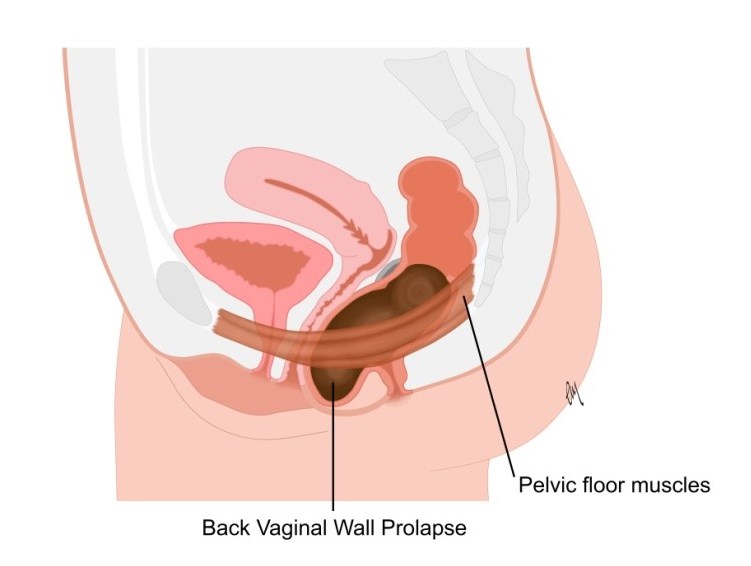
Picture of a posterior wall prolapse (below)
Picture of an apical prolapse (below)
A vaginal prolapse happens when the supporting structures and muscles in the vagina are too stretched or weak to keep the vaginal walls in place. Vaginal prolapse is common in women who have had a vaginal delivery but can happen to any woman even if she has not had children and can happen at any time although prolapse is more usual towards and after the menopause years. The likelihood of having a prolapse rises with age. Other factors such as genetics, obesity and a lifestyle or job that involves heavy manual work or activity can make prolapse more likely.
About a third of women will be aware of bothersome symptoms from a prolapse. The most common type of prolapse is a front wall prolapse –the wall that supports the bladder (see picture).
A prolapse may be mild or quite large and will usually cause symptoms of vaginal heaviness, awareness of a lump or bulge and sometimes discomfort. These symptoms may affect your quality of life sometimes or all the time and you may have good days and bad days – every woman may be differently affected.
Other symptoms can be common with a vaginal prolapse:
- You may have bladder leakage, going too often, up more at night and not feeling empty. Some women find that they go less often to the toilet.
- The most common bowel problem with a vaginal prolapse is a feeling of incomplete emptying and needing to go more than once to complete a bowel movement.
- Penetrative sex can be uncomfortable particularly if the uterus is low in the vagina and the cervix can be felt near the entrance.
Self help / Advice
Treatments that might be offered for a vaginal prolapse are:
- “wait and see” – the prolapse may not get any worse
- pelvic floor exercises – to strengthen the vaginal support system (link to PF section)
- lifestyle changes – including weight loss, good bladder and bowel habits and appropriate exercise (link to lifestyle section of healthy PF habits)
- a vaginal pessary - an internal device that is placed into the vagina to support the walls that have dropped downwards
- surgery – to repair the stretched vaginal walls and lift them back into place. Surgery does not work for everyone and may need to be repeated. It may not improve bladder symptoms if they were not caused by the prolapse.
Every woman has a choice of what treatment might be best for her at any given time. Current guidelines recommend non-surgical treatment options should be tried before surgery is offered.
In the first instance:
- try to avoid activities that make the prolapse symptoms worse such as high-impact exercise, prolonged standing, repetitive bending or heavy lifting
- eat healthily to avoid constipation and ‘hard to pass’ bowel movements
- consider doing your pelvic floor exercises in a lying position so that the vaginal walls are not on strain
- you may want to join a prolapse support group online to understand that you are not alone in having this problem
- make sure that you have kept up to date with cervical screening smear checks
- download or read POGP booklets
Where to go to next
If your prolapse continues to be bothersome refer yourself or ask to be referred to a physiotherapist with specialist knowledge of pelvic health. (link to find a physio)
You may want to see your GP particularly if you are experiencing vaginal dryness or discomfort. You might benefit from treatment with vaginal oestrogen and the use of a lubricant for sex. Your GP may refer you to see a specialist doctor (urogynaecologist/ gynaecologist).
Useful links for further information are:
What to expect from physiotherapy
The specialist pelvic health physiotherapist will ask in detail about your symptoms, and what you have tried already. You will be asked if you are happy to be examined, so that the physiotherapist can examine and measure your prolapse and to discover what type you have, as well as assess your pelvic floor muscles . If your pelvic floor muscles are weak, you will be taught how to strengthen them correctly. The physiotherapist may examine you whilst you are standing up.She may also refer you to another healthcare professional for further treatment such as a vaginal pessary device or consideration of surgery if that is your choice.
More About Physiotherapy Assessment