Good Bowel Health
Explanation of common symptoms/ problems
Good Bowel function is really important to feel healthy; when things aren’t working well it very quickly has an effect on our quality of life.
Anal incontinence it can affect anxiety and willingness to go to new places, try new things or even meet up with friends in public. It can also affect the type of job you choose and the bonding you have with your family and partner.
Bowel or anal incontinence (AI) refers to the unwanted leakage of flatus or stool from the bowel. It can be made worse due loose stool. AI can occur after childbirth due to birth trauma especially with regards the anal sphincter – 3rd or 4th degree tears. It can also become a symptom around the menopause and later years due to hormonal changes and reduced strength in the pelvic floor and surrounding support structures. It can also be associated with neurological disorders and spinal injury.
At the other end of the scale constipation can make us feel uncomfortable, painful and sluggish. It too can affect our quality of life if each bowel movement ‘takes hours’ and gives us no satisfaction of completeness and feeling empty.
Constipation can also have an impact on worsening prolapse symptoms, the onset of bladder symptoms and can aggravate persistent pelvic pain.
Bowel function can change for many reasons including:
- Stress
- Postnatally due to birth trauma
- With change (e.g. when you go on holiday, routine, medication, diet)
- Following surgery
- Presence of a prolapse
- Slow food transit
- Dehydration
- Irritant foods
- Irritable bowel syndrome
- Bowel cancer
However, there should never be more than a drop of visible blood on opening your bowels and sudden changes in ability to pass stool or stool type, as well as the onset of abdominal pain especially after eating should be discussed with your doctor.
In an ideal world stool should be firm but not hard and easy to pass and you should not need to strain. Stool like this is often easier to ‘hold on to’ and therefore less likely to leak or smear.
Self help / Advice
- Start regular pelvic floor muscle exercises
- Eat little and often and try not to miss breakfast! Try to have something every 2-3 hours to keep your gut regular, avoiding very long gaps between meals. Three meals and three snacks are ideal, making sure that these snacks are nutritious. Avoid snacking on processed foods, cakes, biscuits, crisps or foods high in fat and/or sugar.
- Fibre is important for a healthy bowel and forming a good stool consistency. Some foods contain fibres that soften your stool while other foods contain fibre that gives your stool bulk/substance. The goal is to eat a balanced amount of each to achieve a stool that is smooth, formed and easy to move!
- If your stools are hard, dry and sometimes difficult to pass eating food such as kiwis, pears, plums, dried fruit, prune juice and green vegetables may help.
- If your stools are loose, soft or mushy then foods such as wholegrains, spelt bread, milled linseed/flaxseed or psyllium husk supplements may help by adding bulk to the stool if you trial including them in your diet.
- Gradually increase fibres over 3-5 days to reduce risk of stomach discomfort or excess wind.
- Fibre needs fluid to be effective regardless of your stool type. Make sure you are getting in at least 1.5 – 2 litres daily, the majority of which should ideally be water.
- These are basic dietary suggestions. For more specific individual advice speak to a Registered Dietician or gastroenterologist, possibly via referral from your GP.
- Try to never ignore the urge to move your bowels or put it off for very long. Going regularly can often prevent accidents later on. It is very easy for this to happen if you are distracted with work or caring for children
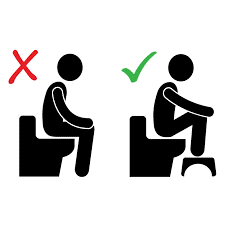
- We often feel the urge to go shortly after eating or exercise. Be aware of these urges and don’t ignore them where possible. Sit well on the toilet, relax and do not hover! If possible, put a small footstool or step under your feet to lift the feet/knees. Relax, lean forward, keep your tummy soft, breath normally and do not strain.
- Ensuring good/regular fluid intake
- If constipation is difficult to manage and nothing works even when you do everything right, it is important to talk to your doctor.


- Daily exercise helps to promote regular bowel activity and benefits your overall health. Aim for 30 minutes of exercise at least 5 days of the week. Walking is a simple way to get moving but do try to find something you enjoy. Jogging, swimming, cycling, pilates or yoga are all good options too. Taking time to exercise is also good for your mental health, can aid in stress management or can just give you some time to yourself.
- Regular mindfulness practice has been shown to be beneficial in gut health. Maybe try some meditation, mindfulness apps or online relaxation videos. As little as 10 minutes each day has been shown to have benefits for physical and mental health.
Where to go to next
If you are still bothered by regular constipation, especially if you think you may have a prolapse please speak to your GP who may be able to prescribe some laxatives in the form of softeners or medicines to bulk your stool; for short or long-term use. You could also ask for a referral to your local women’s health physiotherapy service.
If you are still struggling with faecal leakage despite regular pelvic floor exercises, please speak to your GP who will refer you to your local women’s health physiotherapist and urogynaecologist or colorectal team. They may do further investigations to assess the anal sphincter complex for damage following a vaginal birth.
What to expect from physiotherapy
A specialist pelvic health (women’s or men’s health) physiotherapist can help guide you with correct food and fluid intake - trying to avoid common irritants. They may also be able to help with the triggers that are causing the problems; for example helping with stress and anxiety management, giving support on how to manage changes in diet with travel. With this they may be able to give you tips and tricks to add in to your daily routine to ease bowel opening. A specialist physiotherapist can also help with specific exercise plans to reduce bowel urgency as well as strengthening the pelvic floor complex, containment products and other products to aid bowel opening when relevant.
They may also be able to refer directly into their local multidisciplinary team including gynaecologist, urogynaecologist or colorectal services.