Bowel Dysfunction in Children & Teenagers
Explanation of common symptoms/ problems
Constipation is a common cause of bowel dysfunction in children and teenagers and can also contribute to bladder symptoms.
Constipation can cause your child to poo less often, and they might be hard and uncomfortable. They might have more regular bowel motions, but which are difficult to empty fully. Also, they might have poo accidents (soiling) as a result of not going regularly or emptying well.
By the time a child is 4 years old they should have a bowel routine similar to adults, which means that it would be normal to have a poo anytime from three times a day up to three times a week.
Problems can occur due to an underlying medical condition or unintentional changes in routine as a result of pain; fear or anxiety; what they are eating and drinking; or changes e.g. starting nursery or changing school. Simple habits like ignoring the urge to go for a poo or embarrassment due to previous accidents or being scolded may result in problems.
Self help / Advice
Once you have discussed these symptoms with your GP/healthcare provider and have ruled out any underlying issues which may need further tests or treatment, the following advice may be helpful:
- Understanding normal bowel function is the key to retraining your child’s symptoms. Our digestive system and bowel like a routine of calm and regular filling and comfortable, complete emptying.
- We can encourage this by eating the right foods and eating ‘little and often’. A diet well balanced with enough fibre, fruit and vegetables will help. Talk to your child/teenager and see what they are happy to eat, choose vegetables they enjoy or blend up into sauces if they are not keen! Soft fruits (such as pears, plums, kiwis) or dried fruit (prunes, apricots, raisins) are good snacks. Nutritious snacks also help to avoid any long gaps between meals and keeps the digestive system moving.
- A child should drink enough fluids, ideally water, spread throughout the day. A good estimate of intake would be 30ml for every kg your child weighs. Perhaps have times/situations throughout the day that are reminders to have a cup of water or drink from their water bottle. Using a star chart or rewards system may help.
- Establish a daily routine of sitting on the toilet to try and have a poo. After breakfast is a great time to start. If they aren’t successful in the morning try again after each main meal, up to three times a day.
- Make the bathroom a positive place. Remove any fear or shame, try to make it fun and light-hearted. Have star charts or tick charts to see progress, perhaps with weekly rewards for following the plan. Reward the effort of following the routine not the action of pooing.
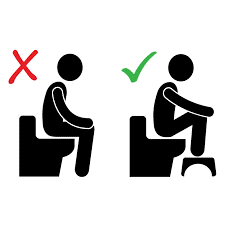
- Encourage your child to sit well on the toilet and use a footstool under their feet if possible. Take their time, breath into the tummy and do not force or strain, try to just relax in this position initially, only pushing when they feel there is a poo there to pass. If it’s a bit uncomfortable or difficult to empty it can be made easier by blowing, singing or try funny noises as they push e.g. ‘mooing like a cow’ or ‘hissing like a snake’. These strategies help to relax the stomach and pelvic floor muscles! If there is no sign of movement after 10 minutes or so, leave it for now.
- Remind them to use this strategy at school or anywhere they may need to go. Try to remove any fear they might have toilets outside of the home or worry about asking to use a toilet at school. Remind them it’s normal to go regularly and everyone does it!
- For girls, make sure they know to wipe from front to back after a wee or a poo.
- Reinforce to your child/teen that it is never a good idea to ignore the urge to go. So, if they feel an urge to have a poo outside of this routine try to find and use a toilet as soon as possible. Don’t put it off.
- It may help to speak with any teachers, sports coaches etc. to ensure the child is free to use the toilet whenever needed.
- Encourage them to be open about any poo accidents or soiling and discuss what they are to do when this happens e.g. having a change of pants, carrying wet wipes. Try not to talk about it as bold, dirty or lazy and don’t punish the child. It is not their fault. It is often useful to refer to these as ‘leaks’ rather than ‘accidents’ and deal with them in an open and practical way.
Where to go to next
It is important that your child or teenager is assessed to rule out any underlying medical causes that may require further tests or treatment. If constipation or bowel symptoms continue to be bothersome you should discuss this with your GP, if you have not already, as they will have a lot of information to offer. They might suggest medications (such as laxatives to ‘clear out’ the bowel), they may require some further tests, or your GP may refer your child/teenager to see a specialist doctor (such as a gastroenterologist or colorectal doctor).
You can also ask to be referred to a physiotherapist with specialist knowledge of paediatric pelvic health for assessment and management of bladder and bowel symptoms.
Find a Physiotherapist
You might find some more information through some of these sources:
What to expect from physiotherapy
- The specialist pelvic health physiotherapist will ask in detail about the symptoms, and what treatments you may have tried already.
- They will explain what seems to be causing the problems and what strategies may now be useful.
- In order to have a more specific assessment of the problem they may ask you to fill in a diary with your child/teen to look at details such as what they are eating/drinking, how often they go the toilet, what the stool looks like, and if there any accidents/leaks, usually over a one or two week period. This will allow the physiotherapist to prescribe individualized strategies to help improve the symptoms.
- They will probably ask about toilet habits, positions or routine and talk about how these fits in with the day at school, after-school activities, sports etc.
- They may also ask about the bladder and any urinary symptoms, leaking or bedwetting.
- If needed the physiotherapist may also have a look at your child/teen’s tummy, if they are happy to be examined. Occasionally they might ask to have a look at the movement of the muscles around the bottom. This might help to teach your child how to ‘let go’ or empty properly, or perhaps learn how to hold on a little better depending on what they need. This will only be done if necessary and with you, and your child’s, full consent.
- You will go home with advice, strategies to improve the symptoms, and maybe some exercises to do; and often will come back to see the physiotherapist with some charts showing how you all have been getting on.
- Further strategies such as breathing exercises, abdominal massage or hands-on techniques, pelvic floor muscle and sphincter retraining exercises, biofeedback, rectal balloon training or other exercises may be discussed on an individual basis depending on your child/teen’s specific assessment.