Other musculoskeletal symptoms in pregnancy
Explanation of common symptoms/ problems
Pregnancy can be a wonderful experience, but it also means your body changes a lot. Sometimes these changes put extra pressure on joints and muscles and can cause you to get musculoskeletal symptoms which could be uncomfortable or even painful. They are most likely to affect you in the third trimester but, in some cases, they can happen in the first or second trimesters or continue after giving birth.
Lower back and pelvic pain are the most common symptoms, but other symptoms may include:
- Neck pain and stiffness
- Thoracic pain and stiffness
- Shooting pain, pins and needles or numbness into the arms or legs
- Carpel tunnel syndrome- pain, pins and needles or numbness in the wrists and hands
- De Quervain's- pain into the base of the thumbs
- Hip, knee, ankle and foot pain, stiffness or swelling
There are lots of reasons why you may experience these symptoms which could include:
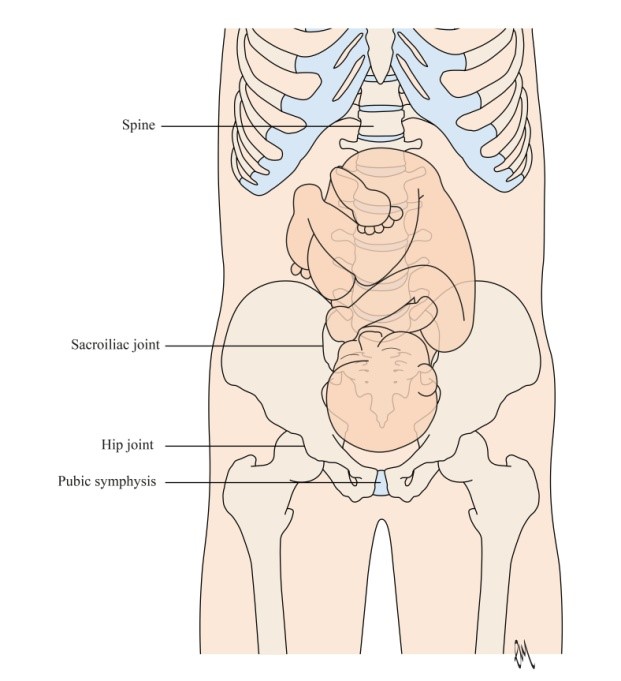
- Changes in the posture of your spine as your baby grows
- Your ‘core’ becomes weaker as muscles stretch and your baby grows
- Hormones being released to allow your joints to become more flexible
- More fluid circulating around the body puts pressure on joints and can also cause you to lose your balance
- Changes in your balance due to the extra fluid and changes in posture
- Enlarged breasts due to milk production
- Feeding your baby in a poor posture
- Lifting, bending and carrying after you have given birth to your baby
- Being overweight
- Spending too much time on your feet
- Spending too much time sitting, especially in poor postures
- Injuries you already had before becoming pregnant
- Poor posture and muscle strength before becoming pregnant
- The more pregnancies you have
Self help / Advice
Although these problems are common, they are not normal and should not be ‘put up with’ in silence. It is important to seek help if you suffer with any new musculoskeletal symptoms as they can be improved with the right advice. See your GP or midwife and ask them to refer you to a specialist women’s health physiotherapist.
For a small number of women there will be a different cause for their pain which needs urgent medical attention. If you experience any of the following:
- Pain going down both legs at the same time,
- Numbness in both legs at the same time,
- Difficulty passing urine,
- Leakage of stool from the bowel that you couldn’t control
- Numbness around the vaginal or back passage
- Dizziness, double vision or black outs
- Numbness in both arms at the same time
- Unusual, severe and persistent headaches or light headedness
- Legs giving way for no reason
- Changes in speech or swallowing
Call your GP straight away or go to your nearest A&E department.
Lifestyle changes can also help your joints and muscles. Simple changes in your lifestyle can have a big impact.
- Try to avoid doing anything too strenuous such as lifting, bending or twisting.
- Where you need to lift something, or someone, such as your baby, try to remember to keep your back straight, bend your knees and keep the load close to you. Try to squeeze your pelvic floor muscles and pull your tummy muscles in towards your spine as you lift and avoid holding your breath.

- Try to pace yourself through the day so that you do things for shorter periods of time before resting or changing the activity.
- If you need a rest, you may want to lay down or sit with your feet up to help your circulation.

- Try to keep a good posture when you are sitting, standing or walking.
- Try to avoid repetitive actions with your arms, hands and wrists. This will help reduce strain on your joints.
- Ensure you have a supportive bra throughout your pregnancy and after you have given birth.
- Exercise is healthy during pregnancy but make sure you are doing exercise that feels comfortable for your body. You will want to adapt exercises the further into pregnancy you go and may want to stop high impact exercise such as running or jumping as these put more pressure on your joints.
Where to go to next
It is important to ask for help if your symptoms do not improve with the advice given here or if you are struggling with sleep and daily activities. Speak with your midwife/ GP in the first instance. They should advise you to see a specialist pelvic health physiotherapist who is trained to treat musculoskeletal problems in pregnancy. You can also contact the POGP who may be able to help find a specialist physiotherapist where you live.
Find a Physiotherapist
Other good sources of information are:
What to expect from physiotherapy
Physiotherapists who treat pregnant women have specialist training and they are used to treating people who have these problems. They will carry out a thorough assessment to find out why you are getting these symptoms and explain what can be done to help improve them. They will make sure that the treatment is very specific to your symptoms.
Your muscles help to support your joints. Research has shown that exercises done alongside lifestyle changes are the most effective way to help improve symptoms of musculoskeletal problems. Your physiotherapist will guide you through a program of exercise and advice to help your specific symptom. In most cases symptoms will improve after you give birth.