The Menopause
Explanation of common symptoms / problems
The menopause is not a disease or illness but a natural stage in a woman’s life when she stops having menstrual periods. This happens when the ovaries no longer release an egg each month and production of the hormone oestrogen declines. This usually occurs between the ages of 45-55 but can be earlier either naturally or after surgery to remove the ovaries or with certain treatments.
The perimenopause or menopausal transition refers to period before the menopause. It may be when you first start to experience menopausal symptoms due to hormone changes but are still having periods. For some women the perimenopause may only a few months but for others it can be several years.
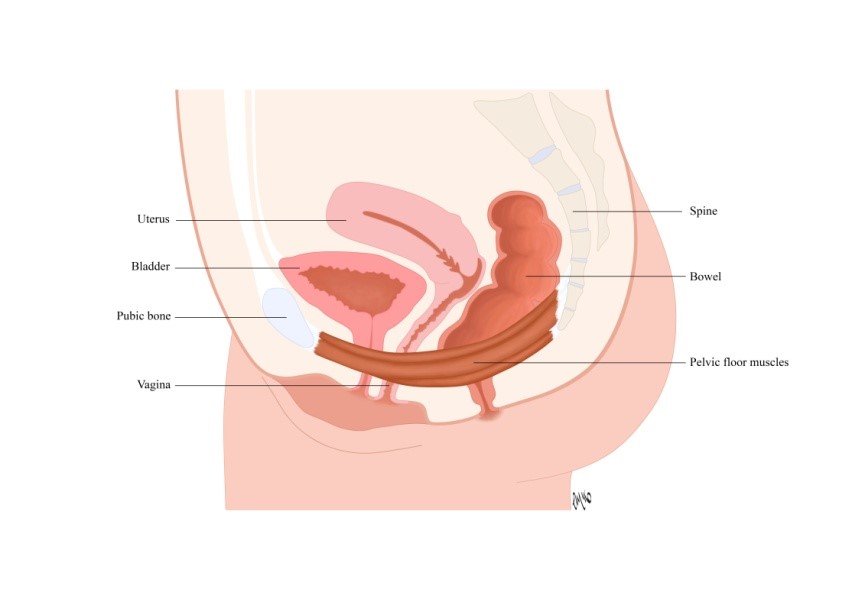
Structures within the pelvic area for example, the vagina, vulva, urethra, bladder and pelvic floor muscle are all responsive to changes in oestrogen levels. As a result, as oestrogen levels drop the following changes can occur;
- Tissues become thinner
- Tissues become less elastic or flexible
- Less lubrication causing vaginal dryness
- Ligaments and muscles less supportive
- A rise in pH – the vagina becomes less acidic
- Change in the balance of “good“ bacteria and “bad” bacteria in vagina
Each woman’s experience of the menopause is different. As hormone production by the ovaries start to fall most women do experience some kind of symptoms, although the type and extent of these can vary widely. The falling levels of oestrogen can lead to a group of genital and urinary symptoms that are called genitourinary syndrome of the menopause or GSM. Some of the symptoms of GSM you may notice include;
- Itching, burning or discomfort in the vaginal area or when emptying your bladder
- Vaginal examinations or smear tests become uncomfortable. If you are still using tampons these
- Light bleeding after sex or vaginal examinations
- More frequent infections of the urinary tract (UTI) and or vaginal infections
- Symptoms of prolapse (see prolapse section for details)
- Increased frequency and urgency to empty your bladder. You may have to rush to the toilet or get up more than once at night. Sometimes may leak before you get there known as urge incontinence (see incontinence section for more details)
- Leakage of urine if you cough, sneeze, laugh or move suddenly known as stress urinary incontinence (see incontinence section for more details)
- The changes in the tissues make them more fragile so penetration can cause small tears and you may also experience bleeding after intercourse
You do not have to have all of these symptoms to be diagnoses with GSM. Many women may experience GSM but few seek help. This may be due to embarrassment, thinking nothing can be done or not realizing your symptoms are even related to the menopause. But you do not have to resign yourself to living with these symptoms as with the right advice and treatment they can be improved.
Bone health during the menopause
Bone health during menopause
Self help / Advice
Depending on your particular symptoms things that could help;
For vaginal symptoms;
- Washing – Avoid any scented products washing this area as they can irritate and make itching worse. Even soap can be drying so water or using an emollient is better. Over washing can also make symptoms worse by altering the natural balance of bacteria
- Clothing – wearing natural fibres like cotton next to the skin and avoiding tight fitting clothes may help
- Vaginal moisturizer- can be used daily. Many different ones are available to buy over the counter. (Different products contain different ingredients so one that may suit one woman may not suit another)
- Lubricants- can be used during sexual activity (as with moisturizer different brands contain different ingredients which may cause irritation)
Do regular pelvic floor exercises
If you have vaginal prolapse symptoms see advise vaginal prolapse section
If you have frequency, urgency or incontinence see advise in incontinence section
Other useful resources;
Where to go to next
If you continue to struggle with your symptoms speak to your GP / healthcare professional. They can discuss whether a topical (local) oestrogen, which has to be prescribed, is appropriate for you. They may also refer you to a specialist doctor (urogynaecologist / gynaecologist)
If your symptoms are related to pelvic floor dysfunction, ask to be referred to a specialist pelvic health physiotherapist.
What to expect from physiotherapy
A pelvic health physiotherapist has specialist training, so they are able to treat women with pelvic floor dysfunction associated with the menopause.
More About Physiotherapy Assessment
Gentiourinary syndrome of menopause (GSM)/ Vaginal atrophy/ Atrophic Vaginitis
Gentiourinary Syndrome of Menopause (GSM)/ Vaginal Atrophy or Atrophic Vaginitis is often described by women as a feeling of vaginal dryness. Genitourinary syndrome of menopause is caused by a decrease in estrogen production. Estrogen is a hormone that increases blood flow to the tissues which gives them stretch; enables strength and helps produce healthy vaginal bacteria. Less estrogen makes your vaginal tissues thinner, drier, less elastic and more fragile. It is estimated that at least 50% of women suffer from GSM but only 7-10% seek advice.
Genitourinary syndrome of menopause (GSM) symptoms:
- Vaginal dryness
- Vaginal burning or burning with urination
- Vaginal discharge
- Genital itching or pain
- Nerve pain in the vulva
- Bladder urgency and frequency
- Recurrent urinary tract infections
- Urinary incontinence
- Decreased vaginal lubrication during sexual activity
- Light bleeding after intercourse
- Discomfort with intercourse
- Vaginal heaviness and symptoms of prolapse
- Physical changes of the clitoris, labia, vagina, urethra and bladder
- Shortening and tightening of the vaginal canal
When to see a doctor
Make an appointment with your doctor if you have any unexplained vaginal spotting or bleeding, unusual discharge, burning, soreness or if you experience painful intercourse that's not resolved by using a vaginal moisturiser.
Causes
Age, surgery or medications that stop estrogen production or the effects of estrogen on the body cause GSM. The menopause or perimenopause is the most common factor that causes GSM but some women experience symptoms when breast feeding; some medications like antihistamines, contraceptive pill, endometriosis treatment or treatment for some types of breast cancer or surgical removal of both ovaries. It needs to be recognised that it maybe undiagnosed in the elderly. A factor other than age and genetics which may contribute to GSM, is cigarette smoking. It affects your blood circulation, and may lessen the flow of blood and oxygen to the vagina and other nearby areas. Smoking also reduces the effects of naturally occurring estrogens in your body.
Vaginal dryness can lead to significant vaginal discomfort at rest; on activity; when having a smear or during intercourse. Although the condition is common, not all menopausal women experience GSM. It is a myth that regular sexual activity, with or without a partner, can help you maintain healthy vaginal tissues.
Genitourinary syndrome of menopause increases the risk of:
- Vaginal infections. Changes in the acid balance of your vagina make vaginal infections more likely.
- Urinary problems. Urinary changes may include increased frequency or urgency of urination or burning with urination. Some women experience more urinary tract infections or urine leakage (incontinence).
Advice:
- Discuss topical vaginal estrogen in the form of a cream or pessary or vaginal ring with your GP. They are often very appropriate to use but you may find they are messy to use and may take up to six weeks to be beneficial.
- Discuss the options for hormone replacement therapy (HRT)
- Follow good vulvar skin care using skin cleansers not soap and consider a vulvar moisturiser with non-perfumed ingredients “If it irritates don’t use it”.
- Avoid removal of pubic hair
- Avoid use of intimate wipes as they may irritate
- Ensure toilet paper and sanitary products do not have added perfume or chemicals
- If using a pad for leakage use an incontinence not sanitary pad as they may keep your skin wet
- Ensure your washing powders/ liquids and fabric conditioners are non-irritating
- Avoid wearing tight clothing and thongs and wear breathable materials for athletic activities
- Use a silicone or hyaluronic lubricant regularly and for sexual intercourse
- See your pelvic health physiotherapist on exercises for your pelvic floor
Websites
www.menopausesupport.co.uk
www.mymenopausalvagina.co.uk
Menopause and Bone Health
There is no doubt Menopause is something of a puzzle
Bone is what we call a ‘reactive tissue’ It is constantly being made and remodelled which means it’s re-absorbed and replaced with new bone. We replace our entire skeleton about every 10 years.
Oestrogen, the main female reproductive hormone is a major player in bone formation; the time of most rapid bone loss starts approximately one year before the final menstrual period.
A woman’s experience of menopausal symptoms is personal and individual
What we do know is that you will benefit from
- lots of sleep,
- a good diet
- exercise.
Physiotherapists, as movement experts are well placed to advise you on the best exercise programmes for this period of your life and particularly around maintaining a healthy bony skeleton.
There may also be other symptoms which act as a barrier to exercise such as symptoms of leakage from the bladder when you exercise or a feeling of heaviness in the vagina. The physiotherapist specialising in pelvic health can help and advise you
The three main components of exercise for bone health (and many other aspects of health) are:
- Resistance training for your muscles
When we contract muscles, they pull on our bones and we know this is very good for healthy bones.
- Plyometric exercise or exercises which increase speed, endurance, and strength, will also help your bones.
- exercises which improve your balance are important as it helps to prevent you from falling and hurting your bones
Starting with small steps the physiotherapist can advise you on a programme of safe exercises.
World meopause day 2021 infographic
You can ask your GP if you can be referred to a physiotherapist at your local hospital or GP practice
Checkout our Physiotherapy directory to find a pelvic health physiotherapist in your area at here
Further information about the Menopause and Bone Health can be found at here