Persistent (or chronic) pelvic pain
Explanation of common symptoms / problems
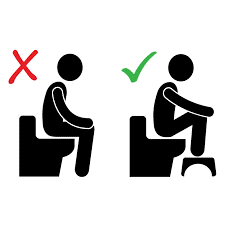
The pelvic floor muscles are the supportive muscles that fill the lower part of the pelvis and surround the bladder opening, vagina and bowel. These muscles tighten to control the bladder and bowel preventing incontinence and relax to pass urine or stool.
We can work the pelvic floor muscles without realising, causing over activity of the muscle, increasing muscle tension, discomfort and preventing relaxation. The overactivity of the muscles causes us to be more aware of any discomfort which causes more tension and symptoms of fatigue, tightness, weakness, cramping, aches and pain in the pelvis and can affect the function of your bladder, bowel and vagina.
Watch: “Why things hurt”
Pelvic pain can be increased with sexual intercourse; stress or anxiety or following a vaginal examination/investigation (e.g. a cervical smear test). There is evidence that symptoms are linked to conditions
Common bladder symptoms
- frequency
- nocturia,
- urgency,
- Incomplete emptying resulting in a constant ‘drip’ leakage or slow flow
These symptoms may make you think you have a urinary tract infection; it is important to provide a urine test to your GP (and only take antibiotics if an infection is found. If the sample is negative and it is likely that the over activity of the muscles that is causing the symptoms, this is bladder pain syndrome (previously known as interstitial cystitis).
Many people with bladder symptoms try to manage the problems by drinking less. This causes concentrated urine and constipation which can irritate the bladder further.
- Make sure you are drinking one and a half to two litres of clear fluid each day.
- If you feel some foods make the bladder pain worse, it may be worth you avoiding these foods for a time to assess if they affect your symptoms.
Also try to:
- Avoid smoking cigarettes
- Avoid drinks that contain caffeine or stimulate the nerves, these include blackcurrant juice, tea, coffee, green teas, fizzy drinks, also chocolate and alcohol.
When you experience urgency there is often a desire to clench your legs together or rush to the toilet. It is often better to relax and after the initial strong sensation of urgency has passed, walk to the toilet at your normal pace.
Bowel Problems
Good bowel health
If constipation is difficult to manage and nothing works even when you do everything right, it is important to talk to your doctor.
Painful sex symptoms
Painful sex is called dyspareunia and you may feel upset when you are unable to enjoy sex with your partner. You may find your skin is sensitive at the opening of the vagina; find it difficult to insert a tampon or have deep pelvic pain during intercourse. Pain can often cause the muscles to tighten without control. If you are a woman who experiences pain during intercourse a lubricant should be used that is paraben free. If you experience pain with intercourse explain to your partner that it may be helpful to limit penetrative intercourse until the muscles improve and changing the position for intercourse may help.
Pelvic pain symptoms
Pelvic pain can come on at any time, sometimes wake you at night; may go down into your legs and your skin may feel sore and isn’t helped much by pain medications. Pain maybe constant or intermittent; a general ache or stabbing and may increase with exercise or walking. When you feel pain regularly it can affect your emotions and you may feel it’s a struggle to cope. It is common for anyone with longstanding pain to have problems with poor sleep, fatigue, anxiety, low mood, nausea, sweating, dizziness or faint feelings. Learning to manage stress and anxiety with relaxation, mindfulness and yoga can help symptoms.
Self help / Advice
If we have bladder or bowel problems, we often think doing pelvic floor muscle exercises will benefit, but they may not be appropriate and could increase pain and symptoms. With such a variety of symptoms identified above it is often a combination of making changes to your lifestyle and muscle relaxation and stretching exercises that can help you to manage chronic pelvic pain.
Where to go to next
What to expect from physiotherapy
Your pelvic health physiotherapist will be able to assess your symptoms and suggest suitable activities to manage each person’s pain and their symptoms.
More about Physiotherapy Assessment