The Prostate
Introduction
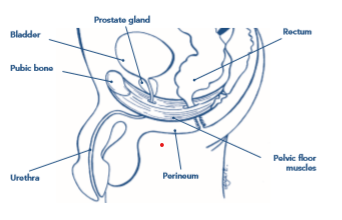
The prostate is a small gland about the size and shape of a walnut that sits below the base of the bladder and close to the urethral sphincter (the valve that keeps you from leaking urine). It also sits close to the pelvic floor muscles.
Most men will have an enlargement of their prostate with increasing age, and this can cause problems such as not being able to empty the bladder as easily, resulting in the need to go to the loo often to empty small amounts of urine at a time. This is called ‘benign prostatic hyperplasia’ or ‘BPH’ and may be treated with medications and sometimes surgery to reduce the size of the prostate in order to make the urine flow more easily.
In some cases, cancer may develop within the prostate gland. Most cases occur in men over the age of 50. One in every eight men will be diagnosed with prostate cancer in their lifetime in the UK. The risk is higher for men whose father or brother have had it, and men of black ethnicity. Men at higher risk may develop prostate cancer before the age of 50. Although prostate cancer is the most common cancer in men, it has a high cure rate if it is detected early.
Explanation of common symptoms/ problems
Prostate cancer and BPH have the same symptoms in common: getting up a lot at night to pee, going to the bathroom more frequently during the day, having difficulty getting started and then having a slow stream, urgency to get to the bathroom and dribbling of urine.
If you have these symptoms you should see your GP so that he/she can best manage your symptoms. A blood test that looks for an antigen known as PSA can be taken. A high PSA may be a sign of prostate cancer and if your test returns a high PSA you may have a biopsy and/or MRI scan.
There is a wealth of information provided by the charity Prostate Cancer UK. Follow this link for further information on all aspects of prostate cancer:
https://prostatecanceruk.org/prostate-information
Recently diagnosed with prostate cancer?
Depending on the stage of your cancer, a decision for ‘watchful waiting’ may have been agreed so that there is no active treatment that you will need to undertake in at least the short term. Others will also have been offered surgery. The surgery will vary according to the hospital trust and surgeon. You may have surgery with or without the assistance of a robot; it may be performed using a laparoscope through your abdomen or be open using a larger incision through your abdomen. Sometimes due to unforeseen circumstances during the surgery, the surgeons will have to make a quick decision to change their planned operation to a different technique to give you the best outcome. Some men will also be offered radiotherapy and others hormone therapy. Whatever the plan, you will be given information in advance by your local team.
Your team will also advise you on the issues that men may have following surgery. These include incontinence of urine and erectile dysfunction.
These symptoms may come about because in taking the prostate out, the sphincters and/or nerves may be damaged; the base of the bladder is no longer supported by the prostate; and the pelvic floor may have also lost their support. Your surgeon will use every technique possible to minimise the risks of developing these symptoms.
Incontinence of urine is very common when the bladder catheter (a tube that is inserted in your bladder during surgery and that usually stay in place for a few days post operatively) is removed. Some men find that they leak all the time when the catheter is removed. This usually settles over time. You may experience stress incontinence; urgency; constant leakage; or dribble after emptying your bladder. Medications for both stress and urge incontinence may be used and you should speak to your surgeon or GP about these. It is estimated that less than10% men are still leaking 24 months following surgery, and in these cases an artificial sphincter that is inserted surgically may be considered.
Erectile dysfunction (ED) may also be an issue due to nerves being damaged during surgery. Some men may have mild dysfunction that can be managed with medication and/or a vacuum pump/intra penile injection to gain an erection, whilst a small percentage may have more severe ED and may have an artificial pump inserted surgically. Talking therapy is an option some men may find helpful in coming to terms with any longterm ED.
Self help / Advice
Before or after surgery
If you have bladder symptoms :
- It is important to keep the pelvic floor muscles strong. If you have the opportunity before surgery, start the exercises as soon as possible
- A useful tool in helping you to do your exercises regularly is the Squeezy app available from your phone’s app store.
- You will be able to start these exercises again once the catheter has been removed and you have the go-ahead from your hospital team. Don’t’ worry if you haven’t had a chance to start these before your surgery. If you are struggling with these post operatively, ask your surgeon or GP to refer you to a physiotherapist who specialises in men’s health.
- It is common to have incontinence when the catheter is removed and you may find that you need to use a protective pad. It is a good idea to buy some of these in advance. Hopefully you won’t need them for too long. Pads are made either as unisex or specifically for men. Unisex pads go under the gusset front to back, whilst the male pads are more of a triangle shape and fit in the front of your briefs without extending underneath you. Whichever pad you chose, you need to have some well fitting underpants. Loose fitting boxer shorts do not keep the pad close to you and you are likely to leak past the pad.
- If you get the opportunity it is useful to discuss medication options for your bladder with your surgeon before you have surgery so that medications can start early if necessary. These will be to help urgency and/or stress incontinence.
If you have erectile dysfunction:
It is very important that you discuss a plan for the management of erectile dysfunction (ED) before you have your surgery if possible so that you have the best possible outcome.
- Prostate Cancer UK recommends that drug management be started for erectile dysfunction from about three weeks post operatively (depending on the protocol of your surgeon) The medication should be tried over a period of time that covers at least 8 attempts at gaining an erection.
- A vacuum pump that artificially creates an erection is also recommended for preventing scar tissue that may otherwise shorten the penis and cause it to retract in the long term. This may or may not be available to you in your Healthcare Trust but they are available commercially
- There is no evidence that pelvic floor muscle exercises can help erectile dysfunction (ED) following prostate surgery but we know they can help men who have ED of unknown cause. Physiotherapists therefore encourage you to do them.
- It is very important to regain and maintain your fitness following prostate surgery. Getting back to the level of exercise that you did before surgery will take some time and you should pace yourself up to this once your surgeon advises that it is safe to do so. If you have not previously had a fitness routine you may wish to address this. If you are carrying extra weight you should consider reducing it. The NHS has excellent resources in helping you to get fit and/or lose weight.
Where to go to next
If you continue to have incontinence and/or ED after three months, or are concerned that you have lost fitness and you have not already been offered physiotherapy, ask your surgeon or GP to refer you to a physiotherapist who specialises in men’s health.
You may also ask to be referred to the team nurse who specialises in the erectile dysfunction specialist nurse and your local continence team for advice on other suitable containment products.
If you develop late effects of radiotherapy that may include chronic fatigue, bowel issues or pelvic pain you should ask your GP to refer you for physiotherapy.
If you feel able to, start trying to increase your fitness levels and drop some weight if you are carrying extra pounds.
If you feel you are of low mood and need some support you should speak to your GP or self refer for talking therapy.
What to expect from physiotherapy
A specialist Men’s Health physiotherapist will listen to you, will answer your questions, work through any concerns that you may have and provide ongoing support
- A full history will be taken as well as an assessment of your pelvic floor muscles.
- A treatment programme will be agreed that may include:
- Prescription of an individualised pelvic floor muscle training programme tailored to your needs
- Bladder training
- Advice with respect to further self management techniques for urinary and/or bowel incontinence and/or ED
- Advice with respect to regaining your fitness
- With your agreement your physiotherapist will liaise with your medical team so that in working together the best possible outcome will be achieved for you