Perineal Healing After Having Vaginal Birth
Explanation of common symptoms/ problems
90% of women giving birth vaginally to their first baby will get a perineal tear. This most often occurs to either the skin at the vaginal opening (labia/vulva) or the tear may be deeper involving the pelvic floor muscles. A few women will also have a tear to the muscles of the back passage. Sometimes the midwife or doctor delivering your baby will suggest making a small cut to one side of the vagina (called an episiotomy) to try to prevent bigger tearing.
If you do have a tear to the muscles of the vagina and back passage, this is called a third or fourth degree perineal tear. Six out of 100 women giving birth to their first baby will have this type of tear.
Most of the time the stitches that you have will heal within six weeks of birth without problem. If you have had a third or fourth degree tear you may be aware of the stitches for a bit longer (three to four months after birth).
In the first few weeks after birth there can be problems with the stitches such as:
- Pain or discomfort in the perineum that is preventing you from sitting, walking, carrying your baby comfortably.
- Swelling, bleeding or a smelly discharge.
- Pain on having a bowel movement or passing urine
Other problems that you may have from having a perineal tear are:
- An urgent need to pass urine or stool
- Leakage of urine from your bladder or stool from your bowel
- Difficulty passing urine or stool (especially for the first time)
- Pain during sexual intercourse
- Feeling emotional, anxious, stressed about a difficult birthing experience.
If you do have any of these problems contact your GP, midwife or physiotherapist for advice.
Self help / Advice
Things that you can do to help your perineum heal are:
- Keep your stitches and the surrounding area clean. Wash daily with water only. Change your sanitary towels regularly ( i.e every 3-4 hours or once the pad becomes moderately dirty) Make sure that you wipe front to back when you go to the toilet.
- When passing urine for the first time try to sit and relax on the toilet. Pouring some luke warm water over as you pass urine may be more comfortable.
- When having a bowel movement for the first few times you may wish to wrap some toilet paper around your hand or use a clean sanitary towel to support your perineum. Try to relax on the toilet as much as possible. Placing a stool under your feet and leaning forwards can also help. Having a bowel movement won’t affect your stitches.

- Try not to get constipated. Straining is not good for your stitches, perineum or pelvic floor muscles. Follow the advice on our Healthy Bowel page.
- Use an ice pack made from a sanitary towel for 10-15 mins at a time every 3-4 hours. To make an ice pack dampen a sanitary towel with water and place it in the freezer until frozen. Just be sure to wrap the sanitary towel in a damp cloth and only keep it on for as long as is comfortable up to 15 mins. This is especially good to do in the first day or two after birth.
- Gently squeezing and relaxing your pelvic floor muscles may help pain and swelling. Once the pain and swelling settles it is important to carry out pelvic floor muscle exercises every day to make sure that they work well after birth.
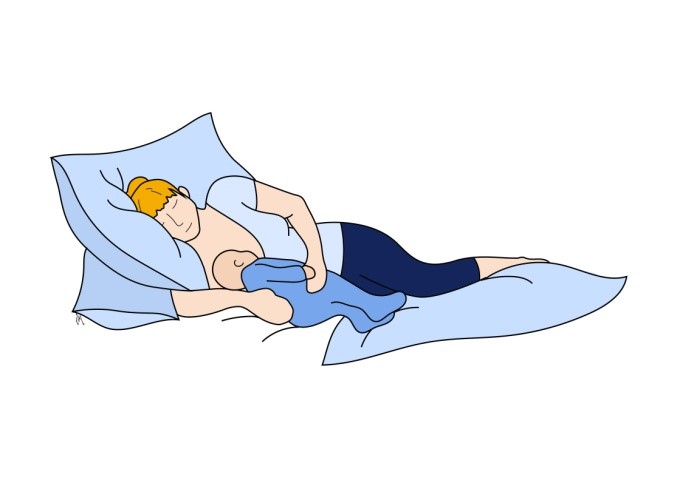
- If you are finding sitting uncomfortable try resting or feeding in a side lying position.

Gradually return to exercise as you feel comfortable. You shouldn’t feel any significant heaviness or discomfort to your perineum after exercising. Start with some short 10-20 minute walks and gradually build up distance and speed. Be careful returning to high impact aerobic exercise too soon, such as running, zumba or cross fit.
Return to sexual intercourse when your wound has healed (at approx. 6 weeks after birth), feel ready and have arranged which contraception to use. Start gently and you may find it helpful to use a water-based lubricant for comfort.
Where to go to next
All women will have a postnatal check with their GP approx. 6-8 weeks after birth. This is to check on your recovery. If you are having any problems with the healing of your perineum, this is a good opportunity to mention it to your GP.
Between 6-12 weeks after birth women who have had a third or fourth degree perineal tear will have an appointment at the hospital with either a specialist doctor, physiotherapist or nurse. At your appointment you will be asked about how you feel your recovery is going and if you are having any problems, particularly with your bladder or bowels. With your agreement the health care professional that you see will check the healing of your perineum and carry out a vaginal and rectal examination to assess how well your pelvic floor muscles are working. They will also suggest things that you should be doing to help with your recovery such as your pelvic floor muscle and anal sphincter muscle exercise. You should have an opportunity talk about any concerns that you have and about any plans that you may have for future births and how your perineal tear may affect this.
If you are struggling with unpleasant thoughts and emotions about your birth you may have the option to speak with health professionals in the Birth Reflection Service. If this is not available to you speak with your midwife or GP so that they can find the right professional to help.
If you are having problems with your bladder or bowels, have any symptoms of prolapse, have scar pain or are struggling to return to sexual intercourse, ask your GP to refer you to a specialist pelvic health physiotherapist. You can also search the POGP directory to find a physiotherapist in your area.
Find a Physiotherapist
For further information:
What to expect from physiotherapy
Pelvic Health physiotherapists who work with obstetric patients have specialist training and they are used to treating people who have these problems. They will carry out a thorough assessment to find out why you are getting these symptoms and explain what can be done to help improve them. They will make sure that the treatment is very specific to your symptoms.
More about Physiotherapy Assessment