Pessaries for Prolapse - Patient Information
Pessary for vaginal prolapse
This section explains what vaginal prolapse is, the benefits and the risks of having a pessary for treatment of vaginal prolapse, and the alternatives to pessaries.
A full version of the content on this webpage is available with useful images in this Information Booklet also available in Turkish
We have answered the most common questions asked by women regarding prolapse and pessaries. However, we do understand that every woman’s situation is different and individual to them and advice from an appropriate healthcare professional is always preferable. If you do have any specific questions, it is important to speak to your own doctor, nurse specialist or physiotherapist for further help.
Already have a pessary?
What is a vaginal prolapse?
Vaginal prolapse is a common condition where the walls of the vagina and sometimes the uterus (womb), or vaginal roof (if you have had a hysterectomy) bulge downwards towards the entrance of the vagina. A vaginal prolapse is also known as a pelvic organ prolapse.
Download infographic PDF Vaginal Prolapse Download infographic PDF Vaginal Prolapse in Turkish
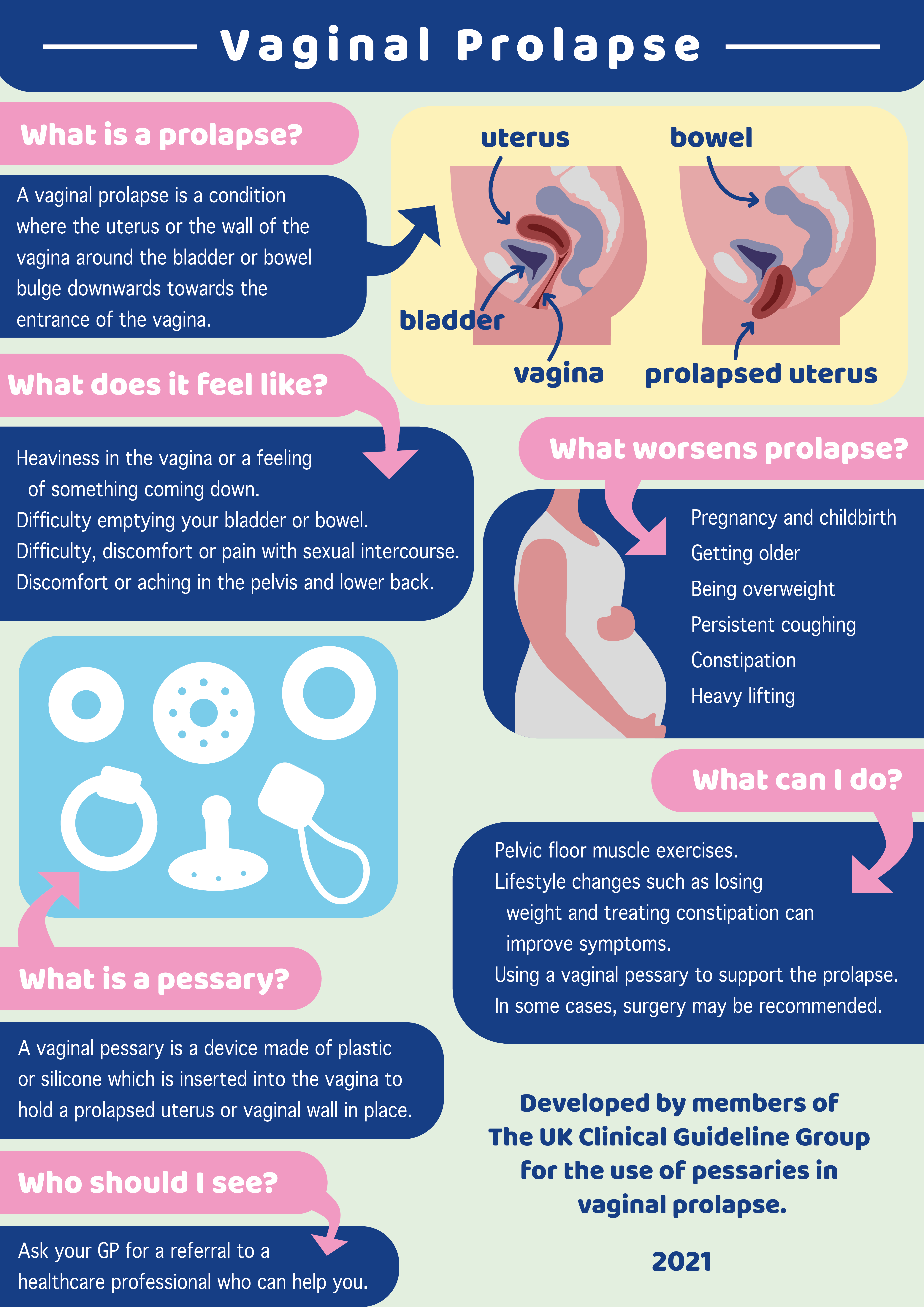
What are the symptoms of a vaginal prolapse?
You could have one or more of these symptoms:
- A feeling of something coming down, a dragging sensation or a bulge in the vagina
- Difficulty emptying your bladder or bowel
- Discomfort/pain during sexual intercourse
- Discomfort or aching in the pelvis and low backache
What increases the risk of vaginal prolapse?
Some women have connective tissue in the body that is more flexible and provides less support than others, so can be more likely to prolapse. This can be aggravated by other factors such as:-
- Pregnancy and childbirth
- Getting older
- Being overweight
- Persistent coughing
- Constipation
- Heavy lifting
What can be done to help improve your symptoms?
- The following are sometimes referred to as 'conservative' or 'non-surgical' approaches.
- Lifestyle changes can reduce symptoms.Losing weight, treating constipation and reducing heavy lifting all reduce the pressure on your pelvic floor muscles. Pelvic floor muscles are shown in the picture below (figure 3). They help to support your pelvic organs – bladder, bowel and uterus.
- Using a vaginal pessary to support the prolapse alongside doing pelvic floor exercises.
- Pelvic floor muscle exercises help to strengthen the muscles and will help improve support
In some cases, surgery may be recommended. Surgery is offered when other non-surgical options haven’t managed to control or reduce your symptoms.
It is recommended that you see a pelvic health physiotherapist before considering surgery for a small or medium sized prolapse.
Click here for more information about pelvic floor muscle exercises
Audio Guide to Completing Pelvic Floor Muscle Exercises
If you have difficulty doing the exercises, are worried that you might not be getting them right or find that your symptoms are not reducing, you can ask to be referred to a pelvic health physiotherapist.
What is a vaginal pessary?
A vaginal pessary is a device, made of plastic or silicone, which is inserted into the vagina to hold a prolapsed uterus or vaginal wall in place. It will also support your bowel and bladder. There are different types of pessaries and the healthcare professional who assesses your prolapse will discuss the type best suited to you. It sometimes takes more than one visit to get the right size, fit and type for you.
What are the benefits of a vaginal pessary?
Once fitted correctly a vaginal pessary may help to reduce your symptoms and make you feel more comfortable. You will be able to continue with your everyday activities including exercising, working and caring for your family.
What are the risks of a vaginal pessary?
There are a few side effects and risks. Your healthcare professional will tell you about these.
You may notice you have more vaginal discharge than normal. If the discharge is offensive see your pessary fitting clinician or your GP.
Occasionally bladder or bowel function could be affected.
You may have vaginal irritation. If you feel sore, and have been through the menopause, you may benefit from using vaginal oestrogen.
Long-term use of a vaginal pessary may cause ulcers (sores) inside the vagina, and/or infection. To reduce the risk of this happening, your pessary should be changed every 4–6 months. You may also be prescribed vaginal oestrogen.
Vaginal oestrogen can be used either as a cream or in the form of a pellet or a ring (also called a pessary) which is inserted into the vagina. The hormone is absorbed by the vaginal tissue and works locally. This means that unlike other hormone replacement therapy (HRT) the amount absorbed into the blood stream and travelling round the body (systemic absorption) is very small. Your healthcare professional will advise you as to which oestrogen is most suitable for you.
Frequently Asked Questions
Who will fit my pessary?
A qualified health care professional with experience in managing pessaries
Can I ask for a female practitioner?
Yes, you can, although there may not be a female practitioner available in every clinic so you may want to make this request in advance of your appointment. You should be offered a chaperone and you may also choose to have someone else with you such as a partner or friend.
Will I get a choice of device, or see what my pessary looks like before it is fitted
Not all pessaries work for all women and all types of prolapse. After you have been assessed, the person who is fitting your pessary should show you which device is most likely to be appropriate for you. They will discuss your options with you, which may include the option of managing the pessary yourself. They will then show you the device, explain how it works and fit your pessary with your consent.
N.B. Sometimes it can take more than one fitting to find the device and size that works best for you. Throughout the process your doctor, nurse practitioner, or physiotherapist will work with you to make sure that you get the best possible results.
How do you know what size to fit? What does it look like?
The person fitting your pessary will have assessed which size pessary is required and will show the pessary to you before it is fitted. Ask to see what it looks like.
What is it made of?
Pessaries are usually made of plastic or silicone.
Will I feel it in place?
No, ideally you should not feel it once it is in place and have a good fit. However, the pessary can move within the vagina, a bit like a tampon, so you may be aware of it at times, but it should not be uncomfortable. The person fitting your pessary will be able to show you what to do If it does become uncomfortable.
Will it fall out when I exercise?
A pessary should not fall out if correctly fitted. There is an element of trial and error when fitting pessaries for the first time, so a pessary could fall out while you are trying different ones. Once you have a well-fitting and comfortable pessary, it will not come out during exercise, but it can still move.
Should I give up my exercise activities?
No. You should be able to continue exercise with a pessary. Many women find they can be more active once they have a correctly fitted device in place.
I have been doing pelvic floor exercises. Should I continue with them?
Yes. It is important to continue with your pelvic floor exercises.
Can I use a tampon?
Yes. You can use a tampon if you have a ring type pessary as long as it feels comfortable.
Will it fall out when I strain to open my bowels?
Supporting the area between the anus and the vagina when opening your bowels gives confidence to push, without pushing the pessary out. Wrap toilet paper or a sanitary pad around your hand and press and support the area just in front of the anus and around the opening of the vagina. Avoid getting constipated.
How often should a pessary be checked or changed?
Depending on which type of pessary you have, this can be every 3–6 months by a healthcare professional. For self-managing pessaries, how often you remove a pessary depends on the type of pessary you were given and personal choice, but it is still important to check your pessary regularly. For pessaries that don’t require removing daily, they can be removed occasionally, for example once a week or a month, though you do not have to do this if you don't want to. As a guide the minimal time for changing a pessary and replacing it with a new one is once every 6 months.
Will I be prone to more vaginal infections?
You may occasionally get a vaginal infection which can be treated with a local antibiotic vaginal cream or by removing the pessary and leaving it out for a while. Oral antibiotic tablets will be given if required.
An infection is less likely if the pessary is changed regularly and the vaginal tissues are kept healthy by using vaginal oestrogen which may be prescribed.
Will it affect my sex life?
It is possible to have penetrative vaginal sex with some pessaries such as a ring or Shaatz pessary, but others would have to be removed first and replaced later. You will be able to discuss with your healthcare professional options of which pessary might best suit you, along with any concerns you may also have about contraception.
How difficult is it to remove and put back in?
Some pessaries can be self-managed. The clinician who fitted your device will assess suitability and discuss this with you and will teach you how to remove it and reinsert it while you are with them in clinic. It is not usually difficult to remove a pessary or replace one once you have been shown how and have practiced.
Can I self-manage my pessary?
Yes. You may be offered self-management of your pessary by your healthcare professional if suitable. You can manage your pessary yourself once you have been shown how to, have practiced and are confident to do so.
Do I need to use lubricants?
You may find it more comfortable to use a vaginal lubricant when inserting a pessary, especially a new one, but you do not have to.
What is vaginal oestrogen and why might I need it?
Vaginal or topical oestrogen is a very low dose of the hormone oestrogen.
Vaginal oestrogen can be used either as a cream or in the form of a pellet (also called a pessary) which is inserted into the vagina and absorbed by the vaginal tissue. This is also available as a ring-shaped device which releases hormone slowly over 3 months. This means that unlike other hormone replacement therapy (HRT) the amount absorbed into the blood stream and therefore traveling round the body (systemic absorption) is very small.
Oestrogen is found naturally in the body and one of its functions is to keep the condition of the vaginal tissues healthy. Oestrogen can be lacking during and after the menopause and it can cause vaginal atrophy. Vaginal atrophy is when the lining of the vagina becomes thin and dry and the skin around or in the vagina can feel sore or itchy. Your healthcare professional will advise you if you need oestrogen and which type will be most suitable for you
How effective will vaginal oestrogen be?
Oestrogen cream can be very effective at making the condition of the vagina healthier and reducing soreness and discomfort and in turn, reducing the risks of infection and ulcers which a vaginal pessary may cause.
Can I expect my prolapse condition to go back to normal after a while or is this it for the rest of my life?
No. Using a vaginal pessary controls the symptoms of a prolapse by supporting it. The pessary will not ‘heal’ or ‘cure’ the prolapse. Sometimes when the pessary is removed, there may be a temporary improvement, but this is not likely to last over time.
Is this currently the preferred treatment for prolapse?
It is one of a small number of choices available for managing vaginal prolapse, but each woman is different and treatment choice varies with each individual. You can change your mind about your treatment at any time.
My friend had surgery and that was fine for her. This was not offered to me as an option. What are my options?
Surgery may be considered but often women are offered a less invasive option to try first as all surgery will carry some risk including prolapse recurrence. Surgery for prolapse may include hysterectomy if the uterus has prolapsed. However, with some surgical procedures women do not need to have a hysterectomy. Removing the uterus itself does not always cure the prolapse and may make other types of prolapses more common.
Can I buy a pessary from my local chemist myself to experiment myself?
It is possible to buy online but it is not advisable without having been assessed by a trained professional who can make sure you have the correct and most suitable pessary. There are a large variety of pessaries on the market and an appropriately trained healthcare professional will be able to help you find one that is likely to help you and your specific prolapse and symptoms. If you buy one online, it would be advisable to ask a healthcare professional to check it is suitable for you before you use it.
What happens if I am self-managing my pessary and it gets stuck?
Don’t panic! It is much easier to remove a pessary if you are relaxed and in the right frame of mind.
Contact the clinic where the pessary was fitted, your GP or go to the nearest A&E.
Self Management of Vaginal Pessary
Information for Women on Self-Management of Pessary for Vaginal Prolapse
Booklet - Information for Women on Self-Mangement of Pessary for Vaginal Prolapse
Download infographic self management of a Vaginal Pessary

To self-manage your pessary, you need to:
- Want to self-manage
- Have the ability and confidence to remove and reinsert the pessary
- Be aware of how to look after the pessary e.g. checking its condition and cleaning the pessary
- Be able to re-order a new pessary or request one on repeat prescription
- Monitor any changes and recognise when help or advice might be needed Removing and reinserting the pessary
The person who assessed you and fitted your pessary will have shown you how to put the pessary in and take it out. Help will be available until you feel confident to do this on your own.
You will be advised how often to remove the pessary depending on the type of pessary you are given.
For pessaries that don’t need to be removed daily there are no hard and fast rules on how long you keep a pessary inserted, but as a minimum it is recommended that you remove it every three months.
There is no harm in removing your pessary and leaving it out for a period of time if you wish to. For example: you could remove it overnight then wash and reinsert in the morning about once a month.
You could just use it for exercise if that is the only time your prolapse bothers you.
You can discuss any questions you have about removing your pessary with the person who
provided you with the pessary.
Cleaning the pessary
You will be advised how to clean your pessary. It usually involves washing with warm water and a mild pure soap. There is no need to sterilise the pessary. Sterilising can have an adverse effect on the material that the pessary is made from. When cleaning your pessary, it is a good idea to check its condition. Look for any cracks or splits in the material that might have appeared or a general change in the pessary’s condition. Discolouration of the pessary often occurs and is not harmful.
Changing the pessary
You will be told at the clinic where your pessary was fitted, whether you should either order a new replacement pessary from the clinic directly or request it on repeat prescription. As a guide the minimum time for changing and replacing the pessary with a new one is once every 6 months.
Tips to help with any changes to your condition
If you have difficulty emptying your bladder or bowel remove the pessary first and once you have successfully passed urine or opened your bowels wash the pessary and reinsert it. If this happens regularly contact your clinician as you might benefit from a smaller size pessary.
Avoid getting constipated
Supporting the area between the anus and the opening of the vagina (figure 5)) when opening your bowels gives confidence to push without pushing the pessary out. Wrap toilet paper or a sanitary pad around your hand and press and support the area just in front of the anus and around the opening of the vagina.
Occasionally a pessary may come out completely and you may need to wash and reinsert it or replace with a new one. If this happens often contact your clinician as you might need a bigger size of pessary.
It is normal for the pessary to move sometimes. This may cause discomfort. If this happens, try moving the pessary back into position.
It is a good idea to have a spare pessary available.
If any of the following symptoms occur, you should contact the clinic or your GP
- Smelly or offensive discharge.
- An increase in discharge is very common but it should not be smelly. If you notice smelly discharge, contact your clinic or GP. You can change pessaries more often to help with discharge.
- Bleeding from the vagina. If this happens, take the pessary out if you are able to and contact your clinic or GP.
- Soreness, discomfort or pain. If this happens, take the pessary out if you are able to and contact your clinic or GP.
We Value Your Feedback