Later Years
Explanation of common symptoms/ problems
Ageing is a natural process that happens to us all. As we age many physical changes occur throughout our bodies. These changes affect the different organs tissues, nerves and muscles including those in the pelvic area which can impact on bladder and bowel function.
In addition, some medical conditions that are more common as we age for example Diabetes, Parkinson’s disease can have an impact on bladder or bowel function. Similarly, certain types of medications for example some antibiotics, antidepressants or diuretics may either cause or make some bladder or bowels issues worse.
If you notice bladder or bowel symptoms start or worsen do not stop taking your medication but discuss this with the healthcare professional who prescribed it to see if there is an alternative available.
Although these changes .can mean that issues related to bladder and bowel function can become more common with aging it does not mean this is something you have to put up with as with the right advice or treatment many symptoms can be improved or resolved.
Some of the changes related to ageing in the bladder include;
- Less able to stretch.
- Increased sensitivity when filling
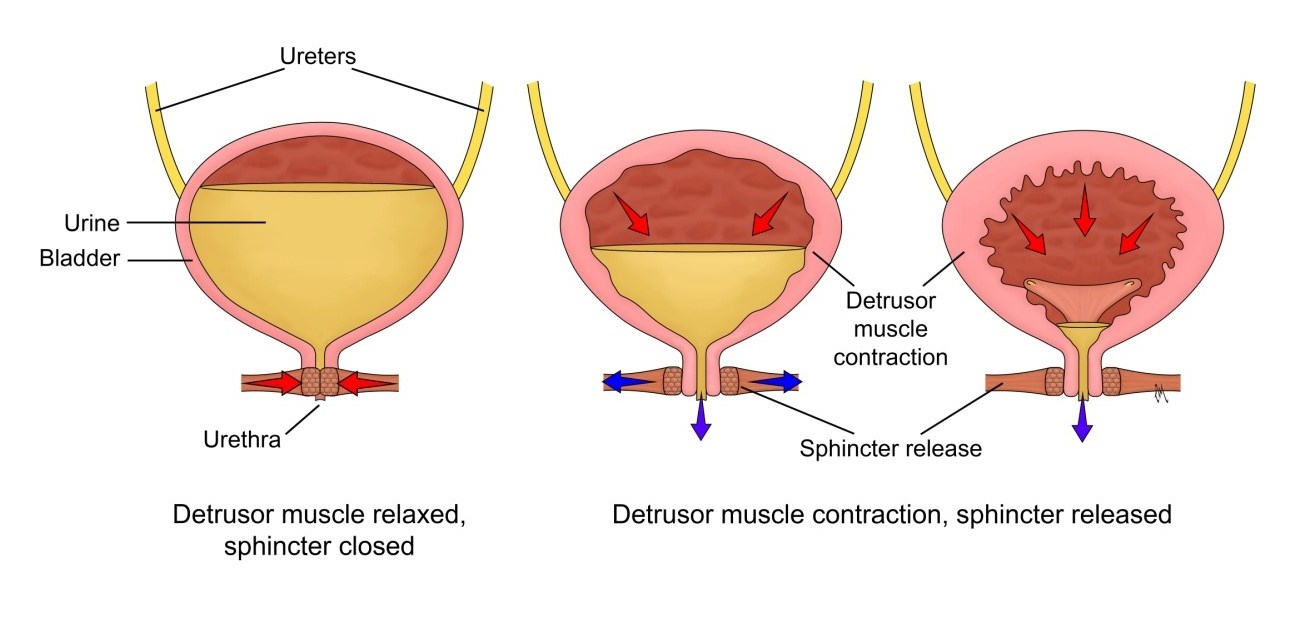
- Detrusor the bladder wall muscle becomes weaker so that the bladder does not always fully empty.
- Changes to the collagen (a protein in muscles and ligaments) resulting in less bladder support
- Weaker pelvic floor muscles
- Decreased production of the hormone antidiuretic hormone (ADH). This main results of this is more urine being produced at night.
These changes can lead to you starting to experience or notice a worsening of one or more of the following symptoms;
- Frequency or needing to empty your bladder more often
- Urgency or a strong desire to empty your bladder that you cannot ignore
- Nocturia or needing to get up more than once at night to empty your bladder
- Urinary incontinence .Depending on your symptoms this can be can either urge incontinence or stress incontinence ( see incontinence section for further details )
- More frequent Urinary tract infections (UTI)
Some of the changes related to aging in the bowels include;
- Changes to the muscles and nerves in the bowel resulting in a slowing of the movement of food waste through the bowel.
- Weaker sphincter muscles that surround the anus
- Change in gut microbiome or balance between “good” and “bad” bacteria that live in our bowels
These changes may mean that you start to experience or notice a worsening of one or more of the following,
- A change in your normal bowel routine - most frequently aging changes can lead to you having your bowels open less often but sometimes you need to go more frequently
- A change in the type of stool you pass. If waste passes too slowly through the bowel stools tend to be hard and difficult to pass. If things move too quickly stools can be too soft.
- Difficulty completely emptying your bowels
- Need to rush to the toilet as soon as you feel the need to empty your bowels
- Bowel incontinence or leaking of wind from the back passage
If you notice a change in bowel routine and /or stool if with any of the following; blood in your stool or bleeding from your back passage, unexplained weight loss, loss of appetite, or fatigue, or pain in lower tummy or when having your bowels open you should see your GP.
Some of the effects of ageing in the vagina include;
- Vaginal walls becoming thinner drier and less elastic .( see menopause section for further details )
- Changes to the collagen resulting in less support to the vaginal walls
- Weaker pelvic floor muscles
These changes may mean you start to experience or notice a worsening of the following ;
- Symptoms of prolapse for example ,a bulge in the wall of the vagina or a dragging sensation in your lower tummy or back ( see prolapse section for further details )
- Itching, burning or discomfort in the vaginal area
- If you are sexually active this may become painful known as dyspareunia. Or you may experience light bleeding after intercourse or even after a vaginal examination.
Any of these symptoms can start to affect your quality of life .You may feel anxious about going out in case you cannot access a toilet or stop taking part in activities you have always enjoyed because you are fearful you may leak. But loss of bladder, bowel or sexual function is not an inevitable part of aging and there are many things that can help prevent or improve your symptoms.
Self help / Advice
Depending on what symptoms are most bothersome to you the following general lifestyle changes may help;
- Top Tips advice
- Good Bowel Health
- Drink well – aim to drink 1.5 to 2 litres fluids spread throughout the day.
- Avoid drinks that can irritate the bladder and trigger your symptoms. These include fizzy drinks , drinks that contain caffeine or acidic juices
- Limit alcohol it not only irritates the bladder but also makes the body produce more urine.
- Avoid drinking a couple of hours before you go to bed.
- Eat Well- have a well-balanced diet. If you suffer with constipation you may need to increase the fibre rich foods such as fruit, vegetables or whole-grain foods.
- Stay active- Doing regular gentle exercise has been shown to have benefits for physical and mental health. It can help directly with pelvic health for example by improving constipation or indirectly by keeping you mobile, so you are able to get to the toilet more easily.
- Do pelvic floor exercises. It is important to do the exercises regularly and correctly if you are not sure about your technique a pelvic health specialist can help.
Other useful resources
Where to go to next
If you experience any of the symptoms described or have tried the lifestyle advice and are still struggling, see your GP and ask them to refer you to a specialist pelvic health physiotherapist.
What to expect from physiotherapy
A pelvic health physiotherapist has specialist training, so they are able to treat women with pelvic health problems associated with the aging process.
More About Physiotherapy Assessment